Foot problems and foot conditions can be a real pain. Whether your foot ailment is chronic or the result of injury or age, poorly designed shoes can exacerbate your foot-related problems and cause unnecessary pain.
At relieffootwear.com, we’re here to help. We are making customised and standardised variety of foot wear products and shoes for problem feet that can reduce pain and prevent unhealthy foot conditions. We strive to educate our guests about common foot conditions and foot problems, while offering a variety of products and shoes for problem feet that alleviate and prevent pain. Whether you suffer from diabetic foot problems, Lymphedema or another foot condition altogether, we can help.
Relief footwear providing wound care and postoperative shoes for diabetics, Front off load footwear, back offloads footwear, Rocker bottom footwear for therapeutic purpose and for preventive factor. We offer diabetic shoes, work shoes, boots, and other footwear that can help diabetics lead full and active lives without fearing for their feet.
Browse our selection of diabetic footwear as per your requirement.
If you have diabetes, whether you work in an office or at a construction site, you’ll need a pair of reliable diabetic work shoes to get you through each day without risking diabetic foot injury. Made from breathable upper materials and solid non skid bottom materials, diabetic work shoes are designed to cushion while providing superior ankle, arch, and heel support, and evenly distributing body weight across the foot to avoid painful pressure points. Diabetic work shoes also provide the extra depth necessary to accommodate custom-orthotics, which can mean the difference between end of the day foot pain and lasting comfort.
For a business casual environment, many men and women prefer to wear diabetic formal and casual shoes. Our Diabetic formal and casual shoes are usually more comfortable versions of popular fashion shoes. relieffootwear.com also sells steel-toed diabetic work boots, for outdoor workers looking for heavy-duty, performance diabetic foot protection.
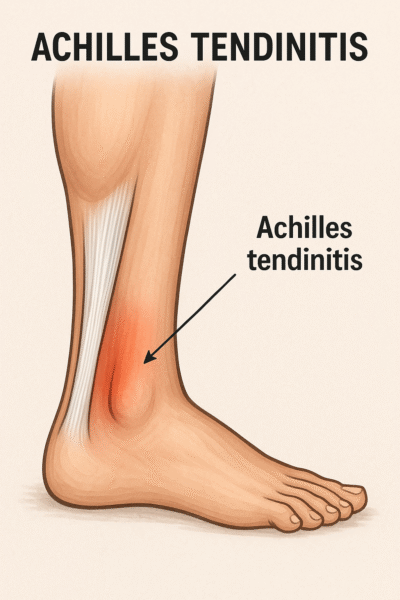
Achilles tendinitis is an inflammation of the Achilles tendon. It is the largest tendon in the body which joins the calf muscle to heel bone and runs down the back of the lower leg.
Heel raised Relief footwear will provide recovery from Achilles tendon inflammation with your every step.
Click Here to order footwear to heal your heel pain.
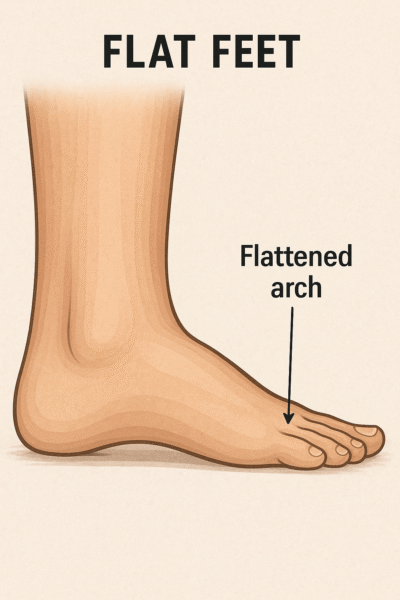
Flat feet (also called fallen arches) is a postural deformity in which the arches of the foot collapse, with the entire sole of the foot coming into complete or near-complete contact with the ground.
There is a functional relationship between the structure of the arch of the foot and the biomechanics of the lower leg. The arch provides an elastic, springy connection between the forefoot and the hind foot so that a majority of the forces incurred during weight bearing on the foot can be dissipated before the force reaches the long bones of the leg and thigh.
Flat feet can affect the alignment of the body when a person is standing, walking, or running. As a result, they can increase the likelihood of pain developing in the hips, knees, and ankles.
Click Here to order medial arch support footwear for your flat foot.

When a foot is exposed to constant stress, calcium deposits build up on the bottom of the heel bone. Generally, this has no effect on a person’s daily life. However, repeated damage can cause these deposits to pile up on each other, causing a spur-shaped deformity, called a calcaneal (or heel) spur.
An inferior calcaneal spur is located on the inferior aspect of the calcaneus and is typically a response to plantar fasciitis over a period, but may also be associated with ankylosing spondylitis (typically in children). A posterior calcaneal spur develops on the back of the heel at the insertion of the Achilles tendon.
An inferior calcaneal spur consists of a calcification of the calcaneus, which lies superior to the plantar fascia at the insertion of the plantar fascia. A posterior calcaneal spur is often large and palpable through the skin and may need to be removed as part of the treatment of insertional Achilles tendonitis.

Diabetes can cause changes in the skin of your foot. At times your foot may become very dry. The skin may peel and crack. The problem is that the nerves that control the oil and moisture in your foot no longer work.
After bathing, dry your feet and seal in the remaining moisture with a thin coat of plain petroleum jelly, an unscented hand cream, or other such products.
Do not put oils or creams between your toes. The extra moisture can lead to infection. Also, don't soak your feet—that can dry your skin.

Calluses occur more often and build up faster on the feet of people with diabetes. This is because there are high-pressure areas under the foot. Too much callus may mean that you will need therapeutic shoes and inserts.
Calluses, if not trimmed, get very thick, break down, and turn into ulcers (open sores). Never try to cut calluses or corns yourself—this can lead to ulcers and infection. Let your health care provider cut your calluses. Also, do not try to remove calluses and corns with chemical agents. These products can burn your skin.
Using a pumice stone every day will help keep calluses under control. It is best to use the pumice stone on wet skin. Put on lotion right after you use the pumice stone.
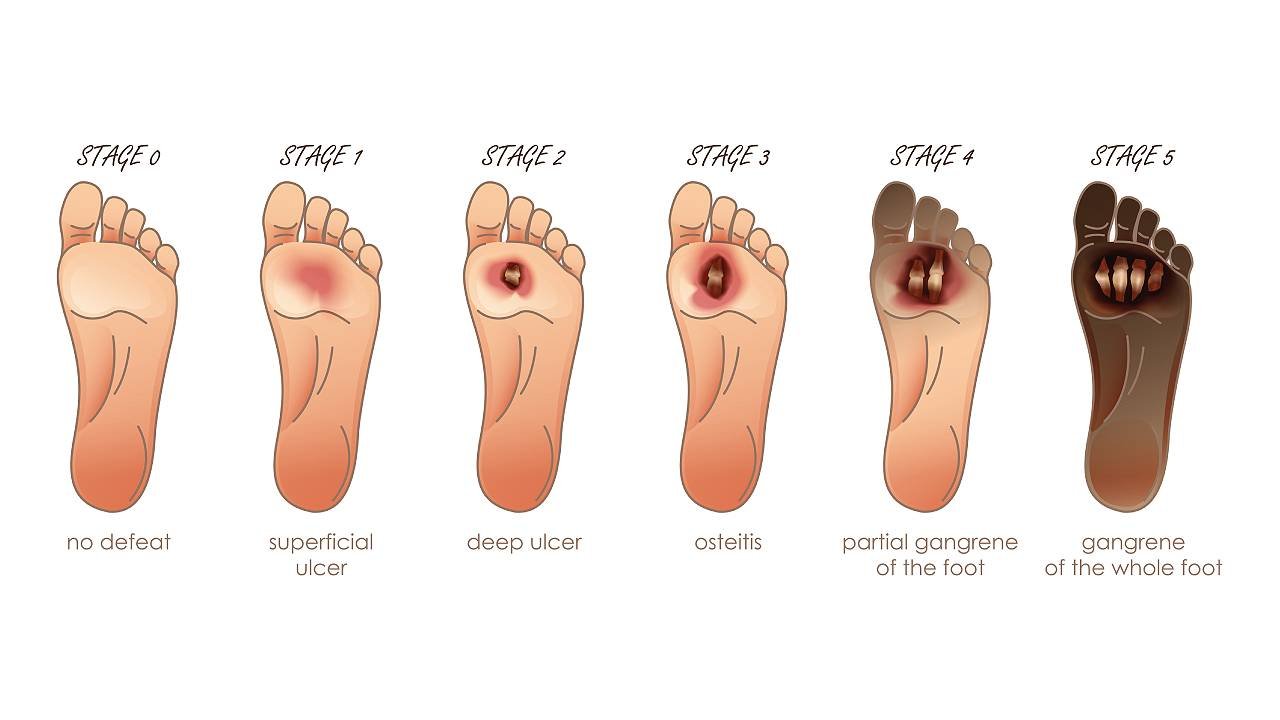
Ulcers occur most often on the ball of the foot or on the bottom of the big toe. Ulcers on the sides of the foot are usually due to poorly fitting shoes. Remember, even though some ulcers do not hurt, every ulcer should be seen by your health care provider right away. Neglecting ulcers can result in infections, which in turn can lead to loss of a limb.
What your health care provider will do varies with your ulcer. Your health care provider may take x-rays of your foot to make sure the bone is not infected. The health care provider may clean out any dead and infected tissue. You may need to go into the hospital for this. Also, the health care provider may culture the wound to find out what type of infection you have, and which antibiotic will work best.
Keeping off your feet is very important. Walking on an ulcer can make it get larger and force the infection deeper into your foot. Your health care provider may put a special shoe, brace, or cast on your foot to protect it.
If your ulcer is not healing and your circulation is poor, your health care provider may need to refer you to a vascular surgeon. Good diabetes control is important. High blood sugar levels make it hard to fight infection.
After the foot ulcer heals, treat your foot carefully. Scar tissue under the healed wound will break down easily. You may need to wear special shoes after the ulcer is healed to protect this area and to prevent the ulcer from returning.
Calluses occur more often and build up faster on the feet of people with diabetes. This is because there are high-pressure areas under the foot. Too much callus may mean that you will need therapeutic shoes and inserts.
Calluses, if not trimmed, get very thick, break down, and turn into ulcers (open sores). Never try to cut calluses or corns yourself—this can lead to ulcers and infection. Let your health care provider cut your calluses. Also, do not try to remove calluses and corns with chemical agents. These products can burn your skin.
Using a pumice stone every day will help keep calluses under control. It is best to use the pumice stone on wet skin. Put on lotion right after you use the pumice stone.
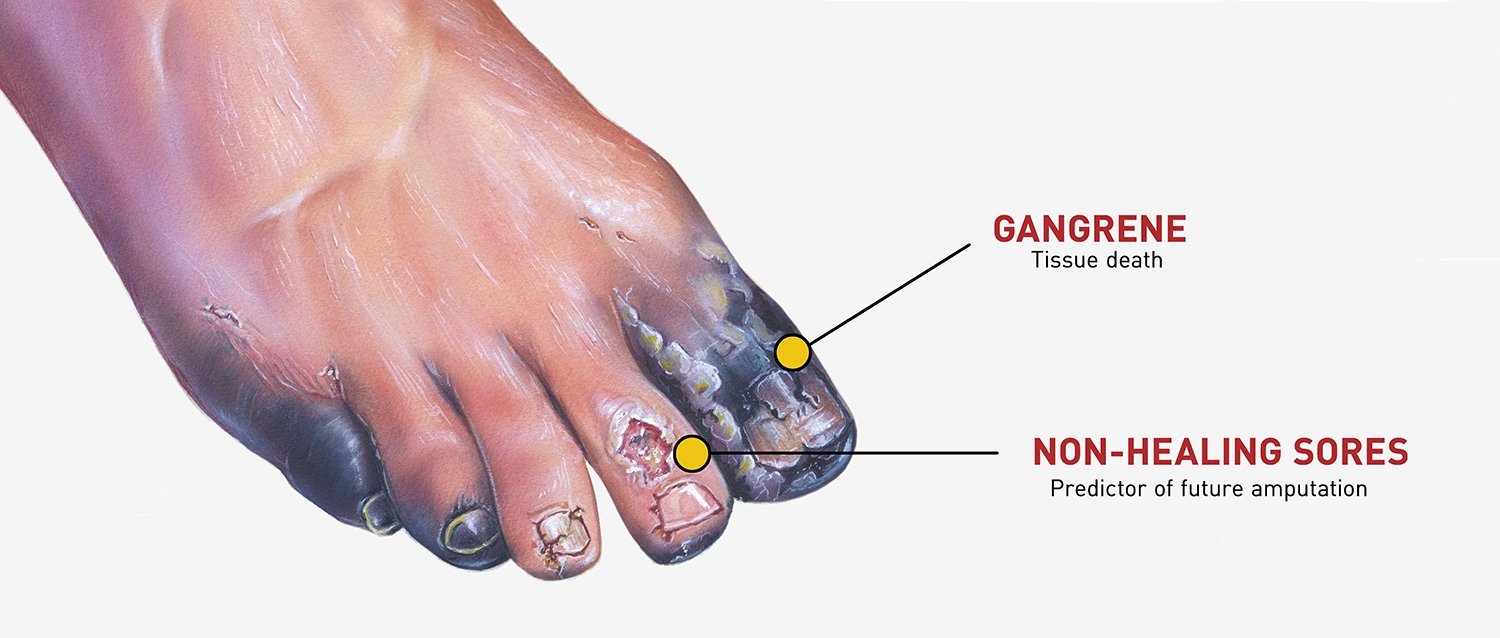
People with diabetes are far more likely to have a foot or leg amputated than other people. The problem? Many people with diabetes have peripheral arterial disease (PAD), which reduces blood flow to the feet. Also, many people with diabetes have nerve disease, which reduces sensation. Together, these problems make it easy to get ulcers and infections that may lead to amputation. Most amputations are preventable with regular care and proper footwear.
For these reasons, take good care of your feet and see your health care provider right away about foot problems. Ask about prescription shoes that are covered by Medicare and other insurance. Always follow your health care provider's advice when caring for ulcers or other foot problems.
One of the biggest threats to your feet is smoking. Smoking affects small blood vessels. It can cause decreased blood flow to the feet and make wounds heal slowly. A lot of people with diabetes who need amputations are smokers.
Athlete's foot is a fungus that causes itching, redness, and cracking. Germs can enter through the cracks in your skin and cause an infection. Medicines that kill the fungus can treat athlete's foot. These medicines come in pills or creams.

Nails that are infected with a fungus may become discoloured (yellowish-brown or opaque), thick, and brittle and may separate from the rest of your nail. In some cases, your nail may crumble. The dark, moist, and warm environment of shoes can help a fungus grow. An injury to your nail can also lead to a fungal infection. Fungal nail infections are hard to treat. Medications applied to the nail are available, but they only help a small number of fungal nail problems. You may need prescription medicine that you take by mouth. Your doctor might also remove the damaged nail.
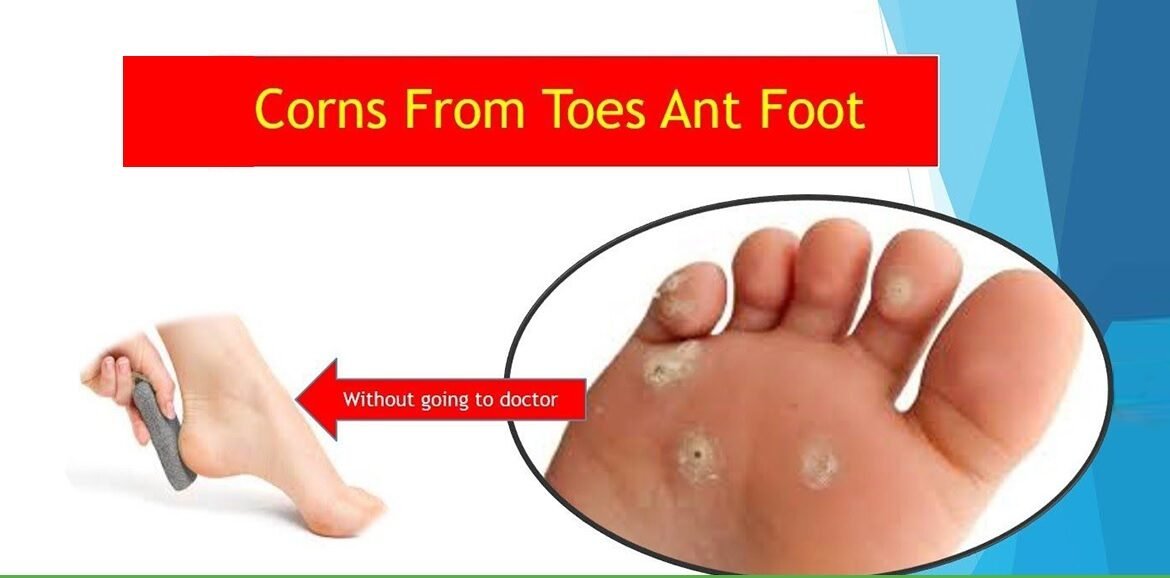
A corn is a build-up of hard skin near a bony area of a toe or between toes. Corns may happen because of pressure from shoes that rub against your toes or cause friction between your toes. Be sure to take care of them properly. After your bath or shower, use a pumice stone to gently remove the built-up tissue. Do not use over-the-counter remedies to dissolve corns. DO NOT try to cut the corn or remove it with a sharp object.
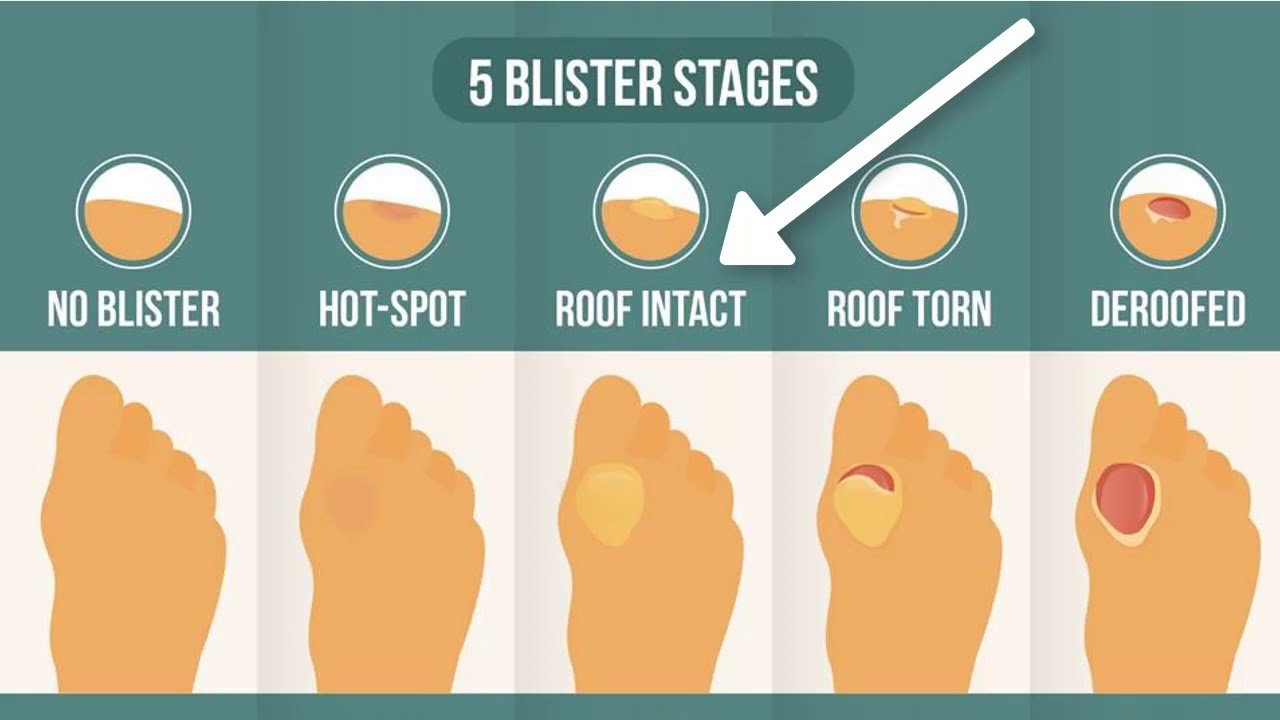
Blisters can form when your shoes rub the same spot on your foot. Wearing shoes that do not fit properly or wearing shoes without socks can cause blisters, which can become infected. When treating blisters, it's important not to "pop" them. The skin covering the blister helps protect it from infection. Use an antibacterial cream and clean, soft bandages to protect the skin and prevent infection.

A bunion forms when your big toe bends toward your second toe. Often, the spot where your big toe joins your foot becomes red and callused. This area also may stick out and become hard. Bunions can form on one or both feet. They may run in the family, but most often they're caused by wearing high-heeled shoes with narrow toes. These shoes put pressure on your big toe, pushing it toward your second toe. Felt or foam padding may help protect the bunion from irritation. Your doctor can also use a device to separate the big and second toes. If the bunion causes severe pain or deformity, you might need surgery to realign your toes.

Dry skin can crack, which can allow germs to enter. Use moisturizing soaps and lotions to keep your skin moist and soft. Ask your doctor which ones to use. Diabetic ulcers . A foot ulcer is a break in the skin or a deep sore. They can become infected. Foot ulcers can happen from minor scrapes, cuts that heal slowly, or from the rubbing of shoes that do not fit well. It's important to treat them as soon as you notice them. Ask your doctor for advice on how to best care for your ulcer. Up to 10% of people with diabetes will get foot ulcers.

A hammertoe is a toe that is bent because of a weakened muscle. The weakened muscle makes the tendons in your toe shorter, causing your toe to curl under your foot. Hammertoes can run in families. They can also be caused by shoes that are too short. Hammertoes can cause problems with walking and can lead to blisters, calluses, and sores. Splints and corrective shoes can treat them. In severe cases, you may need surgery to straighten your toes.

Ingrown toenails happen when the edges of the nail grow into your skin. They cause pressure and pain along the nail edges. The edge of the nail may cut into your skin, causing redness, swelling, pain, drainage, and infection. The most common cause of ingrown toenails is pressure from shoes. Other causes include improperly trimmed nails, crowding of the toes, and repeated trauma to the feet from activities such as running, walking, or doing aerobics. Keep your toenails properly trimmed to prevent ingrown toenails. If you have a persistent problem or if you have a nail infection, you may need a doctor's care. Surgery to remove part of the toenail and growth plate can treat severe problems from ingrown toenails.

Plantar warts look like calluses on the ball of the foot or on the heel. They may appear to have small pinholes or tiny black spots in the center. The warts are usually painful and may grow singly or in clusters. Plantar warts are caused by a virus that infects the outer layer of skin on the soles of the feet. If you are not sure if you have a plantar wart or a callus, let your doctor decide. They have several ways to remove them.